Insurance Claims Processing
|
Innovative Outsourcing solutions to Improve efficiency, accuracy and customer satisfaction
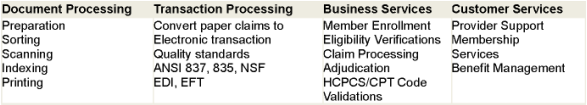
Claim Processing is the single most critical operation for the Payers impacting operational costs and customer satisfaction. Outsourcing of claims administration, adjudication and member services allow Payers to leverage world-class process excellence. Delegating this labor intense operation to transaction processing partner allows Payers to better focus on internal operational cost controls, reduce fraud, adopt innovative technology platforms and most importantly-provide quality customer care. Our BPO solutions provided through a blended model leverage offshore costs with onshore domain functional expertise and deploy best in class training and technology. Our innovative transaction processing services encompass complete spectrum of health plan administration functions built on either client's current technology or our customized claims processing platform. Our solutions dramatically reduce costs and exceed client expectations. Our comprehensive Payer outsourcing solutions include:
Latest Technology
Our qualified service partners deploy leading workflow software platform built on the latest technology infrastructure. In partnership with our client we can customize the application suites to meet client specific needs. Process Excellence Our Service Level Agreement (SLA) assures nearly 100% accuracy level in claims transaction processing. Our Partner Network members are qualified based on maturity with Six Sigma industry best practices, quality certifications and continuous process improvement programs. Compliance In partnership with our clients we ensure that member privacy and data security are maintained through HIPAA compliant processes and encrypted connectivity. Full compliance with the State and Federal Regulations is assured. Domain Expertise Our service partners have deep expertise in the healthcare domain. Trained staff engaged on the Payer claim processing projects typically undergoes extensive industry specific training with US based organizations. |